Progress notes, orders, labs, imaging, plans, and signatures.
Documentation & Coding Engine
Documentation & Coding Engine
Clinical Precision → Clean Claims → Compliant Revenue
Documentation and coding are where clinical truth becomes financial truth. SCIO's Documentation & Coding Engine ensures every encounter is chart-ready, code-ready, and audit-ready—so claims move faster, denials reduce at the source, and revenue integrity stays protected across specialties.
This engine combines clinical completeness checks, coding excellence, and document governance, supported by automation and disciplined quality controls.


Chart Readiness Intelligence
Chart-Complete Before Coding Begins
SCIO's Chart Readiness Intelligence ensures every encounter is fully prepared, validated, and documentation-ready before it reaches coding or billing. Through structured extraction, EMR cross-verification, completeness checks, and intelligent task routing, we eliminate missing notes, unsigned documentation, incomplete orders, and overlooked clinical elements that typically delay coding and trigger payer pushbacks.
By standardizing chart structure and synchronizing clinical + financial documentation, SCIO reduces downstream friction and keeps coding and billing workflows moving.
Smarter chart readiness that eliminates documentation gaps and keeps revenue moving.
What We Do
Clinical data integrity checks
Diagnoses, orders, results, documentation consistency, medical necessity alignment.
Pre-coding readiness audits
High-value/complex encounters validated before coding begins.
Compliance & signature tracking
Unsigned charts, pending attestations, missing provider documentation.
Chart retrieval & document syncing
EMR, portals, fax, digital inbox, and patient records—centralized and complete.
Clinical Coding Intelligence
Coding Accuracy with Compliance Built In
SCIO delivers coding excellence with 98–99% accuracy across oncology, surgical, and multi-specialty practices. Our CPC-certified coding teams apply deep clinical understanding and mastery of ICD-10, CPT, and HCPCS to ensure coding is precise, compliant, and payer-aligned.
To protect revenue and reduce audit exposure, SCIO follows a disciplined 3-tier quality model:
- Self-audit
- Team lead review
- Quarterly compliance audits
The result is fewer denials, cleaner claims, and stronger revenue integrity.

Coding excellence isn't optional—it's the foundation of compliant revenue.
Technology & Controls
- Rule-based validation for ICD-10, CPT, HCPCS, modifiers, and medical necessity.
- Multi-layer QA workflows to sustain 98–99% accuracy.
- Power BI coding dashboards highlighting trends and risks:
- Denial patterns
- Under/over-coded encounters
- Missing documentation drivers
- Provider-specific coding patterns
- Regulatory and payer rule alignment with continuous updates and audits

Document Automation & Governance
From Document Chaos to Audit-Ready Control
Documentation is the hidden bottleneck in RCM—especially with rising payer documentation requirements, medical necessity audits, and specialty workflow complexity.
SCIO's Document Automation & Governance framework streamlines the full document lifecycle:
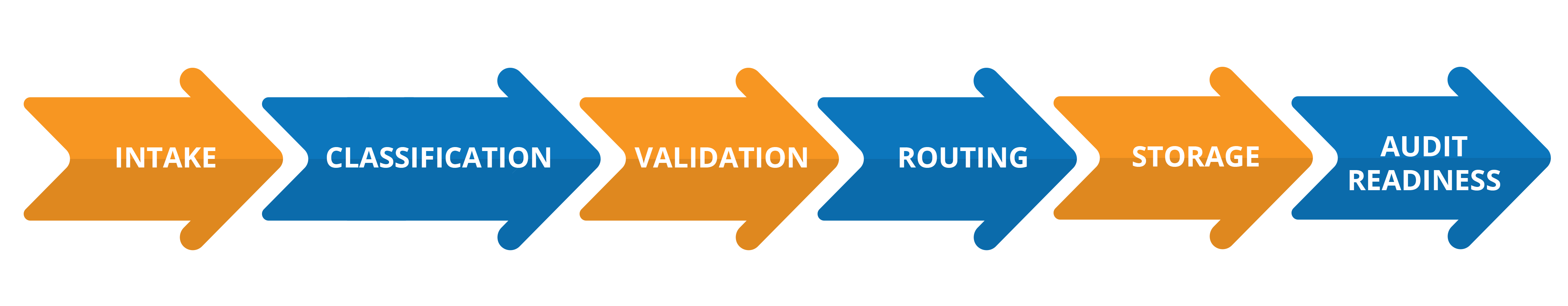
This ensures the right records reach the right teams (Eligibility, Authorization, Coding, Billing, AR, Appeals) at the right time—eliminating delays, preventing missed documentation, and enabling traceable, audit-ready workflows.

Automate the flow. Govern the process. Protect the revenue.
Technology That Powers Governance
- AI document classification (EOBs, clinical notes, labs, operative reports, PA approvals, and more)
- OCR & intelligent extraction (CPT, ICD-10, drug units, DOS, authorization #s)
- Auto-routing workflow engine (Coding, Auth, Charge, AR, Appeals)
- Completeness validation for medical necessity, coding, PA, and claim submission
- Centralized document repository with role-based access
- Provider & payer sync to attach required docs into EMR/PM or claims prior to submission
Operational Outcomes
This is where documentation and coding directly improve financial performance—by preventing issues upstream rather than correcting them later.
- Reduced coding delays through pre-validated chart readiness.
- Higher first-pass claim acceptance with compliant documentation support.
- Lower documentation-related denials through completeness validation and governance.
- Improved audit readiness with traceable document trails and controlled access.
- Faster turnaround across coding, billing, and authorization workflows.
- Stronger clinical-to-billing alignment improving accuracy and payer confidence.

